The New Frontier of Top Surgery: Sensory Nerve Preservation

How a New Approach Is Helping Patients Regain Chest Sensation After Surgery
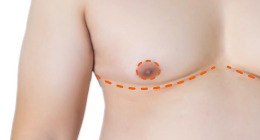
A new approach to double incision top surgery, called sensory nerve preservation, is pushing the boundaries by helping more patients regain chest sensation. Adapted from recent advancements in breast cancer reconstruction, the technique involves carefully preserving key nerves during surgery to support nipple-areola sensation in chest masculinization.
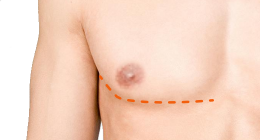
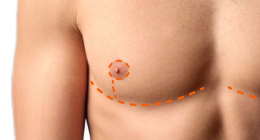
In traditional double incision top surgery with free nipple grafts, the intercostal nerves that supply sensation to the skin and nipple-areola complex (NAC) are cut, leaving the nipple graft and surrounding skin dependent on nerve fibers growing in from the edges of neighboring tissue. This regrowth is slow, unpredictable, and often incomplete.
Sensory nerve preservation (SNP) aims to address this limitation by carefully protecting these nerves during surgery, supporting more reliable and gradual return of sensation to the NAC and surrounding chest skin.
Table of Contents
- Origins: Sensory Nerve Preservation in Cancer Care
- Adapting Sensory Nerve Preservation for Gender-Affirming Surgery
- How Sensory Nerve Preservation Works
- Expanding Access Through Collaboration
- Unlocking the Full Potential of Sensory Nerve Preservation
- Is Sensory Nerve Preservation Right for You?
- Why Surgical Training Matters for Sensory Nerve Preservation
- Surgeons Who Offer Sensory Nerve Preservation
- Resources & Glossary
Origins: Sensory Nerve Preservation in Cancer Care
Dr. Anne Peled, a breast cancer survivor and plastic surgeon in San Francisco, pioneered sensation-preserving mastectomies after recognizing the profound impact that post-mastectomy numbness can have on patients’ lives. Traditionally, sensation was largely ignored in mastectomy and breast reconstruction, with the priority on cancer removal and creating a breast mound. Loss of breast and nipple-areola sensation was considered an unavoidable side effect. Motivated to change this, Dr. Peled, alongside her husband Dr. Ziv Peled, developed techniques to preserve nerves during surgery whenever possible. Since performing her first sensation-preserving procedure, she has completed hundreds of cases and is now teaching other surgeons how to bring this technique to patients worldwide, helping to set a new standard in mastectomy care.
Dr. Peled was first diagnosed with breast cancer at 37, and she recently faced a second diagnosis. She underwent a mastectomy using the nerve-preserving technique she and her husband developed, demonstrating the approach on herself and highlighting its importance in improving quality of life for patients.
Adapting Nerve Preservation for Gender-Affirming Surgery
On the other side of the country, gender surgeon Dr. Jonathan Keith was using downtime from the early COVID shutdowns in New York and New Jersey to develop methods to adapt sensory nerve preservation for gender-affirming mastectomy. “The idea is simple,” he explains, “to reroute the existing sensory nerve to the new nipple in top surgery.” Initially, his team relied on cadaver nerve grafts (allografts), but as the technique evolved, they began to dissect more of the native sensory nerve out of the chest tissue to reach the NAC. Only when the nerve can’t reach the NAC is a cadaver nerve graft used to help guide new nerve growth.
How Sensory Nerve Preservation Works
- Identifying the intercostal nerves that supply sensation to the nipple-areola complex.
- Carefully preserving and mobilizing these nerves during chest tissue removal.
- Rerouting the nerves to reach the new nipple-areola position.
- Grafting if necessary using a cadaver or autologous nerve when the native nerves cannot reach directly.
These surgical steps set the stage for the body’s natural healing response, in which the preserved nerves begin the slow process of reconnecting with the skin. Once the nerves are preserved and positioned beneath the nipple-areola graft, the process of restoring sensation begins. Over time, tiny nerve fibers, called axonal sprouts (extensions from nerves that reconnect with the skin), grow outward from these preserved nerves and seek out sensory receptors in the skin (Meissner’s corpuscles, which detect light touch, and Merkel cells, which detect pressure and texture). If these connections are successful, the graft becomes reinnervated, gradually restoring feeling to the nipple, areola and the surrounding chest area. This regrowth happens slowly, which is why sensation often returns over many months rather than immediately after surgery.
Watch Dr. Keith’s colleague, Dr. Drew Marano, explain how sensory nerve preservation works.
@drew.marano.md Chest and nipple sensation after traditional top surgery methods is unpredictable and often disappointing. Nerve preservation and transfer can increase sensation without adding any extra risk. If you're interested in a consultation, call (201) 449 - 1000 x1021 and ask for Jill to speak to my patient coordinator #genderaffirmationsurgery #genderaffirmingcare #transhealth #transgender #trans #lgbt #lgbtq #plasticsurgery #topsurgery #ftm ? original sound - Drew Marano, MD
Expanding Access Through Collaboration
Meanwhile, back in San Francisco, Dr. Scott Mosser and the Gender Confirmation Center (GCC) partnered with Dr. Ziv Peled to bring double incision top surgery with sensory nerve preservation to patients of the GCC. By this time, Dr. Peled, a board-certified plastic and peripheral nerve surgeon, had performed over 700 sensation-preserving procedures for mastectomy patients. This collaboration allows Dr. Mosser to integrate the techniques pioneered by the Peleds into gender-affirming care, expanding access to patients seeking both chest masculinization and preserved sensation.
While rerouting existing nerves works for most patients, there are situations where the intercostal nerves aren’t long enough to reach the NAC directly. This can happen in patients with higher BMI, larger chests, previous chest surgery, or anatomical variation. In these cases, the regenerating nerves face a gap too large to bridge on their own, which can delay or limit the return of sensation.
Surgeons can address this gap in different ways. Some, like Dr. Keith, have used cadaver nerve grafts to guide new nerve growth. Others, like Dr. Mosser, prefer using nerves harvested from the patient’s own chest tissue (autologous nerve grafts). Unlike oncologic mastectomy, gender-affirming mastectomy often leaves extra donor nerves within the tissue being removed. This difference makes autologous grafting a practical and innovative option in chest surgery for transmasculine patients. In Dr. Mosser’s experience, only about 10% of patients require a graft, with the remaining 90% achieving reinnervation using their native nerves.
Unlocking the Full Potential of Sensory Nerve Preservation
Even with advances in SNP in top surgery, the return of nipple, areola and chest sensation is never entirely predictable. Studies show that most patients who receive SNP report good or excellent sensation within the first year, but these early results don’t capture the full picture.
The research itself has limitations. Follow-up is generally limited to around one year, studies rely on self-reported outcomes rather than standardized sensory testing, and sample sizes in gender-affirming populations remain small. While early gains in sensation are encouraging, long-term comparisons with patients who undergo double-incision top surgery without SNP are still limited. Patients may regain sensation more slowly without SNP, leaving open the question of whether the early advantages of SNP translate into superior sensation over time. Expanding studies and collecting longer-term data could help reveal just how transformative this technique can be for patients.
Is Sensory Nerve Preservation Right for You?
While the research continues to evolve, patients considering top surgery today must still decide whether SNP feels right for them based on their own goals and circumstances. Adding SNP to double incision top surgery adds only about 30 minutes to the procedure and doesn't change overall recovery or increase risks such as neuromas or hypersensitivity. It's a safe addition that can make meaningful chest sensation a realistic possibility for many patients. Still, deciding whether to pursue it involves a few key considerations:
- Importance of sensation: For some patients, nipple, areola and chest sensation after top surgery is highly valued, while for others it may not be a priority compared with chest contour. Sensation can also be a source of dysphoria, making it easy to dismiss during surgical planning. As seen in the patient video below, regaining sensation after surgery can be deeply affirming. Because SNP can't be added later as a revision, this decision must be made at the time of the primary surgery.
- Insurance and cost: As a relatively new technique, SNP isn't always covered by insurers, even when top surgery itself is covered. Out-of-pocket costs can be significant. In Dr. Mosser’s practice, SNP typically ranges from $5,000 to $9,000 USD.
- Anatomical considerations: Patients with higher BMI, larger chests, or a history of prior chest surgery may have intercostal nerves that are too short to reach the new NAC position without nerve grafting, or scar tissue may complicate the process. In these cases, a surgeon may recommend an autologous or cadaver graft, or determine that SNP isn't feasible.
Considering these factors can help patients make an informed decision about whether SNP aligns with their priorities and surgical goals.
Watch LJ describe how SNP helped them reconnect to their chest after top surgery.
Why Surgical Training Matters for Sensory Nerve Preservation
SNP in top surgery is more technically demanding than standard double incision procedures with free nipple grafts. Success relies on the surgeon’s skill in carefully handling and sometimes grafting nerves, which can significantly affect postoperative sensation.
Board-certified plastic surgeons are typically trained in nerve and microsurgery, giving them the expertise to safely handle and preserve nerves during top surgery. Cosmetic surgeons, however, don't receive formal training in nerve or microsurgery as part of their standard education. While they can achieve excellent chest contour, they'd need additional specialized training to safely perform SNP.
Surgeons Who Offer Sensory Nerve Preservation
While surgical training backgrounds differ, what matters most for patients is whether a surgeon has specific experience with nerve-preserving techniques. At present, only a limited number of surgeons routinely perform SNP in top surgery, and availability is concentrated at specialized centers. Below is a list of surgeons known to offer SNP as part of their practice.

Dr. Walter Lin
Dr. Lin is a fellowship-trained Plastic Surgeon in San Francisco who performs Top Surgery. Drawing on his background in microsurgical reconstruction of the breast, he co-developed a novel nerve transfer technique to help preserve chest sensation after Top Surgery. In his 2025 study of 27 patients, the technique proved safe, did not affect appearance, and showed early signs of improved sensation.

Dr. Scott Mosser
Dr. Mosser is a board-certified plastic surgeon in San Francisco with more than 15 years of experience in gender-affirming top surgery. An expert in all major techniques, he was among the first surgeons to introduce sensory nerve preservation for top surgery. He also serves as Medical Director of the Gender Institute at Saint Francis Memorial Hospital.

Dr. Jonathan Keith
Dr. Keith is a board-certified, fellowship-trained plastic surgeon with extensive expertise in gender-affirming surgery. Based in both New Jersey and New York City, he was the first surgeon in NJ to offer the full range of gender-affirming procedures. He performs all types of top surgery and has been at the forefront of developing sensory nerve preservation techniques.

Dr. Drew Marano
Dr. Marano is a board-certified plastic surgeon in New York City specializing in gender-affirming top surgery. He has devoted his career to advancing gender-affirming surgical care while fostering a supportive environment for patients. Dr. Marano has also collaborated with Dr. Keith to expand the use of sensory nerve preservation in top surgery.

Dr. Sarah Eidelson
Dr. Eidelson is a fellowship-trained plastic and reconstructive surgeon with extensive experience in gender-affirming care, particularly for transmasculine and nonbinary patients. Based in Washington, D.C., Dr. Eidelson specializes in masculinizing surgical procedures, with a focus on top surgery with nipple reinnervation.

Dr. Beina Azadgoli
Dr. Azadgoli is a Beverly Hills–based plastic and reconstructive surgeon who provides gender-affirming surgical care for transgender and non-binary patients seeking top surgery. At The Practice Healthcare, she and her colleagues commonly use the Sensory Nerve Preservation technique for both gender-affirming and cisgender mastectomy procedures.

Dr. Nicholas Bene
Dr. Bene is a board-certified plastic surgeon and Director of Gender Affirmation Surgery at Stanford Medicine. He provides the full spectrum of gender-affirming procedures, including top surgery. Dr. Bene trained in gender-affirming surgery through the fellowship program at Oregon Health & Science University, where he learned sensory nerve preservation techniques from Dr. Blair Peters.

Dr. Blair Peters
Dr. Peters is a board-certified plastic and reconstructive surgeon and Associate Professor of Surgery at Oregon Health & Science University. Internationally recognized for expertise in gender-affirming surgery and peripheral nerve reconstruction, he incorporates sensory nerve preservation in top surgery. He has also published invited commentary on SNP, offering a balanced view of its benefits and limitations.

Dr. Lisa Gfrerer
Dr. Gfrerer is an Assistant Professor of Plastic and Reconstructive Surgery at Weill Cornell Medicine. She specializes in gender-affirming top surgery and incorporates sensory nerve preservation to help restore nipple and chest sensation. Dr. Gfrerer has also been the lead author of two important studies on sensory nerve preservation, combining clinical expertise with research to improve outcomes for her patients.
More surgeons who offer SNP:
- Dr. Blair Peters - OHSU, Portland, OR
- Dr. Lisa Gfrerer - Weill Cornell Medicine, New York, NY
- Dr. Katherine Carruthers - Massachusetts General Hospital, Boston, MA
- Dr. Karishma Reddy - Midlothian, VA
- Dr. Javad Sajan - Seattle, WA
- Dr. Krishna Vyas - New York, NY
Advances in sensory nerve preservation have reshaped what patients can expect from double incision top surgery. Where nipple-areola sensation was once considered unlikely to return, SNP now makes it possible for many to regain meaningful feeling in the NAC and chest, often on a faster timeline. Yet outcomes are still variable, and no technique can guarantee a particular sensory result.
Ultimately, the most important outcome of top surgery is the alleviation of gender dysphoria and the ability to live more comfortably in one’s body. SNP represents an exciting advance, but it's one factor among many that shape the overall experience of top surgery. Ongoing research will continue to clarify its long-term benefits and refine the technique. With the right surgeon and an informed decision-making process, patients can choose the approach that best aligns with their goals for surgery and life beyond it.
More Resources:
- Nerve Rehab Guide for Top Surgery
- Research on Sensory Nerve Preservation in Top Surgery
- Top Surgery and Sensation 101
Glossary
| Term | Definition |
|---|---|
| SNP (Sensory Nerve Preservation) | A surgical technique in double-incision top surgery where key nerves supplying the nipple-areola complex are preserved or rerouted to improve the chances of restoring sensation after surgery. |
| NAC (Nipple-Areola Complex) | The nipple and surrounding pigmented skin, which are key areas of sensation in the chest. |
| Axonal Sprouts | Tiny nerve fibers that grow from preserved nerves toward target sensory receptors in the skin, helping restore sensation. |
| Meissner’s Corpuscles | Specialized nerve endings in the skin that detect light touch and texture. |
| Merkel Cells | Nerve-associated cells in the skin that help sense pressure and texture. |
| Allograft (Cadaver Nerve Graft) | A nerve taken from a donor to bridge gaps when the patient’s own nerves cannot reach the NAC. |
| Autologous Nerve Graft | A nerve taken from the patient’s own body to bridge gaps when native nerves cannot reach the NAC directly. |
Last updated: 02/13/26