Drain-Free Top Surgery: Is It Safe?
For many, drains are the most dreaded part of Top Surgery recovery. But can you get Top Surgery without drains? A growing number of surgeons and studies say you can.
In our original article about Top Surgery and drains published in 2016, we explored how post-surgical drains are used to prevent fluid build-up and reduce the risk of complications like seromas, hematomas, and infections. Drains have long been considered “standard practice” for Double Incision Top Surgery, but that standard is changing. Thanks to updated surgical techniques and real-world evidence, many surgeons are skipping drains entirely. Is this safe for patients?
Quick Recap: What Are Drains?
 After surgery, your body produces fluid as part of the healing process. Drains are small plastic tubes that help remove this fluid so it doesn’t build up under the skin, which could cause swelling, pain, or infection. The Jackson-Pratt, or JP drain, is the most common type of drain used for Top Surgery. The JP drain consists of a plastic tube and bulb to collect fluids. While drains can be helpful, they’re not without downsides:
After surgery, your body produces fluid as part of the healing process. Drains are small plastic tubes that help remove this fluid so it doesn’t build up under the skin, which could cause swelling, pain, or infection. The Jackson-Pratt, or JP drain, is the most common type of drain used for Top Surgery. The JP drain consists of a plastic tube and bulb to collect fluids. While drains can be helpful, they’re not without downsides:
- Discomfort and anxiety: Many patients dread the maintenance and removal of drains.
- Infection risk: Drains are a potential entry point for bacteria.
- Scarring: Even when placed through the main incision, some patients report scarring or skin irritation.
- Limited mobility and extra care: Drains can restrict movement and require extra diligence in care.
- Travel and cost burden: Drains must be removed by a professional, requiring patients to stay near their surgeon longer, which increases the overall cost of surgery.
So… are they really necessary?
The Rise of Drain-Free Top Surgery
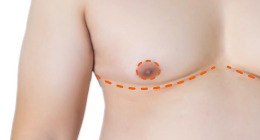
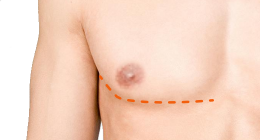
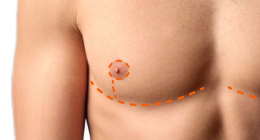
Some surgeons now routinely perform drain-free Double Incision Top Surgery, thanks to a technique called progressive tension suturing. This involves placing stitches inside the chest to close off “dead space” (the open area where fluid might otherwise collect). No dead space means no need for drains!
Two major studies have looked at the safety and effectiveness of this approach, and the results are impressive.
Study #1: Dr. Sidhbh Gallagher’s “Masculoplasty” Technique
Dr. Sidhbh Gallagher, a plastic surgeon in Miami with extensive experience in gender-affirming care, published a study in 2019 of 153 drain-free Top Surgeries using progressive tension sutures. Compared to past studies where drains were used, Dr. Gallagher’s patients actually had fewer complications, including fewer reoperations and shorter hospital stays. Complications included:
- Hematoma (internal bleeding): Just 0.3% of patients
- Infections: 2%
- Seromas (fluid buildup): 0% — none at all
- Revisions (extra surgeries to fix issues): 3%
Dr. Ashley DeLeon
of the Crane Center
Study #2: The Crane Center’s Simplified Outpatient Method
Surgeons at the Crane Center in Texas reviewed 107 patients who had a simplified version of drain-free surgery, done as outpatient procedures. Even though this simpler method had a slightly higher rate of seromas than Dr. Gallagher’s approach, serious complications were rare, and most patients recovered without any issues. The complication rates were:
- Hematoma: 1.9% (only one needed a return to the OR)
- Seroma: 9.3% — but only two patients needed drainage; the rest healed on their own
- Infections & nipple issues: 0%
- Revision rate: 3.7%
The Benefits of Going Drain-Free
Surgeons who use advanced techniques to close off space inside the chest are proving that patients can heal very well without drains, extra scars, or the discomfort that comes with them. Here’s a quick summary of pros and cons of drain-free surgery:
| Benefits | Considerations |
|---|---|
| No tubes, exit wounds, or drain-site scars | Some patients may still get mild seromas |
| Less pain, more comfort | Seromas, if they happen, may need draining |
| Lower risk of hematoma | Not all surgeons offer this technique |
| Easier recovery and care (no draining & recording) | Requires surgeon skilled in this method |
| Shorter compression garment use (~1 week) |
Should You Choose a Drain-Free Surgeon?
If avoiding drains is important to you, then yes, it’s worth asking your surgeon about whether or not they’d recommend them for you. Not every surgeon offers this option, and some still feel more comfortable using drains in certain cases. But the growing evidence shows that, when done correctly, drain-free Top Surgery is safe, effective, and often more comfortable for patients.
Even some surgeons who have historically used drains—like Dr. Scott Mosser—are now leaving the decision up to the patient for certain types of Top Surgery. At the Gender Confirmation Center, drains are still used in most cases, but patients undergoing Double Incision procedures can often opt out. This reflects a shift toward patient autonomy and personalized care, as surgeons recognize that not everyone needs or wants drains.
List of Confirmed Drain-Free Top Surgery Surgeons
These surgeons have published studies, stated their techniques openly, or been verified through patient reviews and clinic documentation as consistently offering drain-free Top Surgery (typically Double Incision with Free Nipple Graft):
- Dr. Curtis Crane & Dr. Ashley DeLeon – Austin, Texas
- Developed a simplified outpatient drain-free method.
- Published study with very low rates of complications, confirming safe, drain-free procedures.
- Dr. Sidhbh Gallagher – Miami, Florida
- Developed the “masculoplasty” technique using progressive tension sutures.
- Published peer-reviewed study with zero seromas and lower complication rates compared to surgeries with drains.
- Dr. Givanni McEvenue – Boca Raton, Florida
- Early adopter of drainless Top Surgery with a large patient cohort.
- Uses techniques based on abdominoplasty-style quilting sutures to eliminate dead space.
- Dr. Alan Dulin, Dr. Scott Harris & Dr. Peter Raphael – Plano, Texas
- Dr. Thomas Satterwhite – San Francisco, California
- Dr. Dustin Reid – Austin, Texas
- Dr. Richard Bartlett – Brookline, Massachusetts
- Dr. Kenneth Wolf – Commerce, Michigan
- Dr. Spencer Eagan – Overland Park, Kansas
- Dr. Gregory Pastrick – Kingsport, Tennessee
- Dr. Daniel Mckee – Vancouver, BC, Canada
What About Penrose Drains?
While many surgeons now offer drain-free Top Surgery, it's important to know that not all drains are the same. For example, Dr. Javad Sajan and Dr. Hope Sherie generally don’t use Jackson-Pratt drains, but they may occasionally place a Penrose drain. This type of drain is soft, flat, and doesn’t involve a bulb or suction. Instead, it allows fluid to passively drain onto gauze. Penrose drains are typically:
- Used only when a very small amount of drainage is expected
- Less noticeable and more comfortable
- Removed within 24–48 hours in most cases
While Dr. Sajan typically performs drain-free Top Surgery, he makes an exception for out-of-town patients who can’t return for frequent follow-ups. In those cases, Penrose drains offer an extra layer of precaution, helping to prevent fluid accumulation during the early days of healing. This proactive approach helps reduce the risk of complications when patients must travel home shortly after surgery.
This video from Dr. Sajan’s realdrseattle series tells the story of Kai, who traveled from across the country to have Top Surgery with Dr. Sajan. At his first post-op appointment, you can see the Penrose drains in place.
If your surgeon mentions using a Penrose drain, know that it’s a very different experience than having traditional post-op drains. It’s still worth asking how long they expect to leave it in and what care it requires, but it’s often far less burdensome than it sounds.
Questions to Ask Your Surgeon:
- Do you offer drain-free Top Surgery?
- What technique do you use to prevent seromas or hematomas if you don’t use drains?
- What’s your rate of complications like seromas or hematomas?
- Have your drain-free patients had good outcomes or required revisions?
- Is there a situation where you’d still recommend drains?
When we first wrote about drains and Top Surgery, we emphasized their role in preventing complications, and in some cases, that’s still true. But surgical techniques have evolved and today many surgeons are proving that with the right approach, drains aren’t always necessary. For patients, that means less pain, fewer restrictions, no post-op drain removal, and one less hurdle on the path to healing.
References
- McEvenue G, Xu FZ, Cai R, McLean H. Female-to-Male Gender Affirming Top Surgery: A Single Surgeon's 15-Year Retrospective Review and Treatment Algorithm. Aesthet Surg J. 2017 Dec 13;38(1):49-57.
- Gallagher S, Rahmani F, Russell A, Duquette S. A Drain-free Technique for Female-to-Male Gender Affirmation Chest Surgery Decreases Morbidity: Outcomes From 306 Consecutive Masculoplasties. Ann Plast Surg. 2019 Jul;83(1):15-21. FULL TEXT.
- Sean A. Knudson, Ashley DeLeon, Curtis N. Crane, Richard A. Santucci. Simplified Drainless Outpatient Female-to-Male Gender-Affirming Bilateral Mastectomy. medRxiv. 2022.06.19.22271559. Note: This is a pre-print and has not been peer-reviewed. FULL TEXT.
- Allure Esthetic. (2021, November 9). Allure Esthetic performs Portland FTM top surgery patients: Dr. Javad Sajan performs drainless top surgery with Oregon health insurance. [Press release]. PR Newswire.
Last updated: 06/19/25