Resources » Top Surgery Journal Articles
Research on Sensory Nerve Preservation in Top Surgery
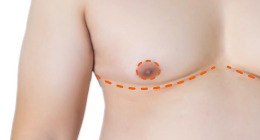
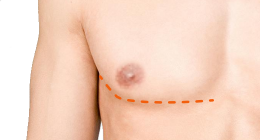
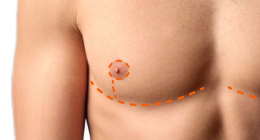
Sensory nerve preservation (SNP) is a surgical technique designed to restore sensation to the nipple-areola complex (NAC) during gender-affirming top surgery. By carefully preserving the nerves that supply the nipple and placing them beneath the nipple grafts, surgeons can help patients retain touch and erogenous sensation that is often lost during traditional double incision top surgery.
Research on SNP is still relatively new, but growing evidence shows that these techniques can significantly speed up postoperative sensory recovery and improve overall patient satisfaction. The studies presented on this page examine how SNP has been applied in both gender-affirming and oncologic mastectomy, and highlight the safety, feasibility, and potential for long-term preservation of nipple and chest sensation.
What's in a Name?
On TopSurgery.net, we use the term Sensory Nerve Preservation (SNP) to describe double-incision top surgery that preserves or restores nipple-areola complex (NAC) sensation. While this is the standard term we use, the same or very similar techniques appear under different names online and in published studies. These alternate terms all describe procedures comparable to SNP.
Alternate Terms
- Reinnervated Top Surgery
- Nerve Preserving Top Surgery
- Sensory Preserving Top Surgery
- Neurotized Top Surgery
- TNR Top Surgery (Targeted Nipple-Areola Complex Reinnervation)
- Nerve Reconstruction Double Incision
- Sensation Preservation Technique / Nerve Reconstruction / Neurotization / re-innervation Top Surgery
- Neurotization for Sensory Preservation
Examples from Studies
- Blair, 2024: Targeted Nipple-Areola Complex Reinnervation (TNR)
- Keith, 2024: Neurotization – Reinnervation of NAC through nerve allografting (cadaveric)
- Gfrerer, 2023: TNR using autologous nerve graft
- Keith, 2022: Neurotized Chest Masculization, using nerve coaptation/anastomosis/connection
- Gfrerer, 2022: Reinnervation, nerve reconnection
- Nguyen, 2021: Neurotization, restoration of sensation, nipple reinnervation
- Nguyen, 2020: Restore sensation, preserving and using specific nerves to reinnervate the NAC
Intercostal Nerve Transfer as a Novel Technique for Sensation Preservation in Gender-affirming Subcutaneous Mastectomy FULL TEXT
This study evaluated whether connecting sensory nerves during top surgery could help restore feeling to the chest and nipple areas. Among 27 patients, the new nerve transfer technique was safe, did not affect appearance, and showed early signs of improved sensation. About half regained nipple sensation within six months, and none developed nerve pain or complications. The authors note that longer-term studies are needed to confirm how consistently sensation can be restored over time.
Invited Commentary: Targeted Nipple-Areola Complex Reinnervation for Sensory Restoration in Gender-Affirming Mastectomy FULL TEXT
This commentary by Dr. Blair Peters discusses Targeted Nipple Reinnervation (TNR) as an exciting advancement in top surgery for preserving nipple and chest sensation. Peters notes that while TNR can improve sensory outcomes, it may not suit every patient’s priorities. Some may value a flatter chest or shorter surgery time more highly. He emphasizes that sensation preservation should be part of an individualized discussion about goals, cost, and access.
Targeted reinnervation during gender-affirming mastectomy with restoration of sensation FULL TEXT
This study examined whether Targeted Nipple-Areola Complex Reinnervation (TNR) can help restore feeling after gender-affirming mastectomy. Fifty patients were included, half receiving TNR and half serving as controls. Those with TNR had significantly better recovery of light touch, temperature, vibration, and erogenous sensation, with most regaining feeling within months. Patients also reported higher satisfaction with nipple sensation and sexual sensitivity.
Direct neurotization of free nipple grafts with cadaveric nerve grafts following mastectomy for gender affirming surgery
This study investigated sensory recovery in patients undergoing gender-affirming mastectomy using nerve allografts to reconnect intercostal nerves beneath nipple grafts. Within one year, 18.5% reported normal sensation and 40.2% minor or diminished sensation; beyond one year, 8.3% had normal and 62.5% minor or diminished sensation. Overall, direct neurotization enhanced sensory recovery compared with standard grafts.
Targeted Nipple Reinnervation in Gender-affirming Mastectomy Using Autologous Nerve Graft FULL TEXT
This study describes Targeted Nipple Reinnervation (TNR) using intercostal nerve branches (T3–T5) to restore nipple sensation. When nerves were too short, tissue from the surgical site was used for grafting. Microsurgical techniques minimized complications. Long-term data collection is underway to evaluate sustained sensory recovery.
Neurotized Chest Masculinization for Improving Nipple Sensation: Survey Results
This survey of 42 patients tested a microsurgical technique to restore nipple sensation. After surgery, about 9.5% reported strong sensation, over half had none, and one-third were satisfied with nipple feeling. Some noted gradual return of sensation within seven months. The method appeared safe and increased the likelihood of regaining some nipple sensitivity.
Targeted Nipple Areola Complex Reinnervation in Gender-affirming Double Incision Mastectomy with Free Nipple Grafting FULL TEXT
This paper introduced a technique preserving lateral intercostal nerves (T3–T5) and connecting them via short nerve allografts beneath the nipple. Nerves were divided into fascicles in a pinwheel pattern to increase coverage. Patients began regaining nipple and chest wall sensation within three months, including erogenous feeling, suggesting the method may enhance long-term sensory outcomes.
Neurotization of the nipple-areola complex: superior nipple sensation in gender-affirming mastectomy and autologous breast reconstruction FULL TEXT
This study assessed nipple neurotization in both transmasculine and reconstructive patients. Lateral intercostal nerves were connected under the dermis of free nipple grafts, improving postoperative sensation across the nipple, areola, and peripheral skin. No patients developed neuromas or hypersensitivity, and sensation was significantly better than in non-neurotized cases.
Immediate Targeted Nipple–Areolar Complex Reinnervation: Improving Outcomes in Gender-affirming Mastectomy FULL TEXT
In ten transmasculine patients aged 16–19, surgeons preserved and reconnected intercostal nerves to reinnervate the nipple-areolar complex. Compared to standard procedures, these patients retained or improved sensation in the nipple, areola, and surrounding skin, with no sensory loss at final follow-up.
Nerve Preservation and Allografting for Sensory Innervation Following Immediate Implant Breast Reconstruction FULL TEXT
Although this study focused on breast cancer reconstruction, it laid the groundwork for sensory nerve preservation techniques in top surgery. Sixteen women underwent surgery with nerve preservation or grafting to reconnect nerves to the nipple and areola. Most maintained light touch and two-point discrimination with no nerve complications. These findings helped shape today’s approaches to preserving sensation in gender-affirming double incision top surgery.
Back to Top Surgery Journal Articles »
Last updated: 11/05/25