Resources » Top Surgery Journal Articles
Top Surgery and BMI: What the Research Shows
Across a growing number of studies on top surgery in transmasculine and nonbinary people, a consistent pattern has emerged: top surgery is generally safe across a wide range of BMIs. Most complications are minor and manageable, and serious events remain rare—even among patients categorized as obese or morbidly obese.
Several studies focus specifically on patients with BMI over 30, a group often excluded from surgery in practice. These findings show that top surgery can be performed safely, with outcomes comparable to those of thinner patients. In some cases, complication rates are no higher at all.
Larger analyses do show that certain risks, like wound healing problems or infections, can increase somewhat at very high BMIs (typically above 40 or 50). But even then, the overall risk of a serious complication remains low. The takeaway is clear: risk should be managed through thoughtful planning, support, and informed consent, not by denying care based solely on BMI.
Don't miss our feature article on Top Surgery and BMI limits.
Association of High Body Mass Index With Postoperative Complications After Chest Masculinization Surgery.
This study examined more than 2,300 top surgery patients to see how BMI relates to complications. Patients with BMI =50 had a much higher chance of at least one complication and urinary tract infections. BMI =35 was associated with higher readmission and surgical site infection rates. Even so, serious complications remained uncommon. The authors suggest rethinking strict BMI limits for patients seeking top surgery.
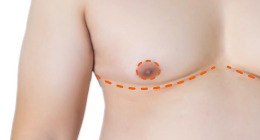
Incidence of Complications in Chest Wall Masculinization for the Obese Female-to-Male Transgender Population: A Case Series. FULL TEXT
Among patients with BMI >30, overall complications occurred in 31.5% of mastectomy sites, most commonly partial NAC loss and minor seromas/hematomas managed in the clinic. No patient required a return to the OR. Notably, those with complications tended to have lower BMI, challenging assumptions that higher BMI worsens outcomes. The authors conclude top surgery can be performed safely on obese patients, and BMI should not be a barrier to care.
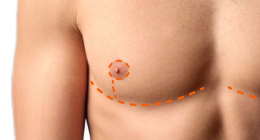
Surgical and patient-reported outcomes following double incision and free nipple grafting for female to male gender affirmation: does obesity make a difference?
In 97 patients (about half with BMI 30–40), complication rates and BODY-Q satisfaction scores did not differ meaningfully between obese and non-obese groups. Complications were low overall, and major events were rare. The authors routinely offer double incision with free nipple graft to otherwise healthy obese patients rather than using BMI to deny surgery.
Gender-Affirming Mastectomy in Transmasculine Patients: Does Obesity Increase Complications or Revisions?
Reviewing 948 patients (˜1/3 with obesity), the study found no significant differences in surgical-site complications or revision rates between obese and non-obese groups, including in double incision cases. The authors advise against using obesity alone to deny surgery and recommend focusing on modifiable risks (e.g., smoking) and surgical technique; more research is needed for the highest BMI ranges (=40).
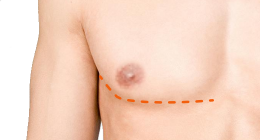
Female-to-Male Gender-Confirming Drainless Mastectomy May Be Safe in Obese Males FULL TEXT
Among 145 patients across four BMI groups (non-obese through “super obese” >50), operative time and tissue resection increased with BMI as expected, but the obese group (30–39.9) did not have significantly higher complication rates than non-obese patients. Higher infection rates were mainly seen in morbidly/super obese groups. Authors conclude delaying surgery for weight loss is generally unnecessary for BMI 30–39.9, and may be considered only at much higher BMIs.
Obesity is not associated with complications or revisions after gender-affirming mastectomy in transgender patients.
In 754 patients followed for an average of 2.2 years, only 7.8% experienced at least one complication. Obesity was not linked to higher odds of complications or revisions. The authors suggest focusing risk discussions on factors like surgical technique and smoking status rather than BMI alone.
Back to Top Surgery Journal Articles »
Last updated: 11/11/25